Stem cell therapy in orthopaedics holds a positive future in treating certain conditions which face a lot of challenges in presently available treatment modalities. These conditions like AVN head of the femur, moderate stage of progressive OA, uncontrolled Rheumatoid Arthritis, Duchenne Muscular dystrophy, etc give enormous challenges to the treating orthopaedic Surgeon. Cell therapy is the most important strategy in the management of the above-mentioned conditions. Defiantly autologous minimally manipulated MNCs should be ideally used. As minimal manipulation is being done so there should not be any safety concern issues. We should plan clinical trials not only from a clinical perspective but also generate sufficient evidence of cellular therapy as treatment options in such conditions. Ultimately angiogenesis and chondrogenesis are required in AVN and OA patients respectively. Hip Avascular necrosis results from interruption of normal blood flow to the femoral head which if diagnosed at an earlier stage, have the option of halting the progression with stem cell therapy. Clinical grade mesenchymal stem cells with or without PRP can be used not only in the treatment of OA but also in chondral lesions due to sports injury. This is the possible correct way to avoid further cartilage degeneration leading to Sec OA. MRI changes post-therapy in AVN, OA must be clinically correlated. The importance of rehabilitation for achieving expected recovery after the therapy must not be forgotten and regular follow-up must be maintained to access the outcomes. Regenerative Science is thus an effective approach based on the unique ability of stem cells to reproduce, repair & rejuvenate the affected damaged tissue.
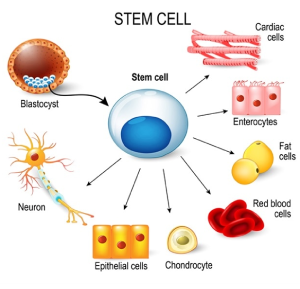
Stem cells are receiving a great deal of scientific attention as well as coverage in the orthopaedic treatment nowadays. One of the many reasons for the attention is the potential of these cells to regenerate tissues without the production of scar tissue. Many new technologies are coming up in orthopaedic management but they are poorly defined with regard to stem cells.
Most of the research aimed at clinical treatments which have been carried out using autologous MSC’s, mainly from bone marrow. Specifically, bone marrow-derived stem cells have been used in vitro to generate bone, cartilage, tendon, ligament, meniscus, intervertebral disc, fat, muscle, and nerve. Because of the availability of adipose tissue, it too has received a fair amount of recent research as a source of MSC’s. A clear delineation of the pros and cons of fat-derived versus bone marrow-derived MSC’s is lacking. Ease of collection procedure, number of stem cells recovered, capacity and efficiency to differentiate into various mesenchymal tissues, as well as morbidity associated with the collection procedure are all important points to consider when discussing bone-marrow versus adipose-derived stem cells. Because MSC’s treatments are being used from both fat and bone marrow, it is important to point out that few direct comparisons have been published, and at this point, a definitive answer is lacking on which population of cells is better. Typically, aspirated bone marrow is described to contain 40 million nucleated cells, of which 2,000 are stem cells per milliliter (or 1 stem cell per 20,000 cells). In contrast, fat is far less cellular (approximately six million cells per cubic centimeter of tissue compared to 40 million in bone marrow aspirates), but the prevalence of stem cells in fat has been described as high as one per 4000 cells, which is higher than that in the bone marrow.
Adult Stem cells & Osteoarthritis
Osteoarthritis (OA) and related degenerative joint disorders have a heavy disease burden and affect millions of people annually around the world. Once damaged articular cartilage lacks the ability to properly repair and regenerate itself. Various surgical procedures are being tried to restore joint functions starting from minimal procedures like shaving after lavage, laser abrasion, microfracture of subchondral bone to more extensive procedures include autologous or allogenic osteochondral transplantation, autologous chondrocyte implantation. The ultimate procedure of total joint replacement remains the treatment of choice today for the extensively damaged joint. Other than total joint replacement above mentioned extensive procedures are effective to various degrees in treating chondral defects of limited sizes. Thus, there is a need for improved cartilage repair modalities.
Adult stem cells, because of the ease with which they can be isolated, their capacity to self-replicate, their ability to differentiate along multiple connective tissue lineages, have become the cell type of choice for cartilage tissue repair. In vivo studies have confirmed MSCs’ ability to localize and participate in the repair of damaged joint structures, including cruciate ligaments, menisci, and cartilage lesions. Most of the in vivo studies utilizing MSCs have focused on meniscal repair, in some cases using MSCs in a carrier or scaffold while in others utilizing direct injection into the joint.
Intra articular technique
The best approach to intra-articular injection is the path having the least obstruction and maximal access to the synovial cavity which could be medial, lateral retro patellar approach or suprapatellar approach, or even anterior (anteromedial or anterolateral) approach. The medial retro patellar approach is frequently being used. The position generally used is supine with the knee flexed to varying degrees. Usually 20/18 gauge sterile needle is carefully inserted into the joint space with an aseptic technique. Advance the needle carefully in the joint space with limited resistances. If there is significant resistance or hitting the bone then one has to again redirect the needle. To prevent damage to articular cartilage do not insert the needle deep. Then syringe having mesenchymal cells is being attached to the inserted needle and fluid is slowly injected in PRP may or may not be injected along with this.
Osteonecrosis or Avascular Necrosis Head of Femur
Avascular necrosis (AVN) of the femoral head can be a devastating progressive disease most commonly affecting patients younger than 40 years of age. Although the exact pathophysiology of AVN has yet to be elucidated, the disease is characterized by a vascular insult to the blood supply of the femoral head, which can lead to a collapse of the femoral head and subsequent degenerative changes. If AVN is diagnosed in the early stages of the disease, it may be possible to attempt surgical procedures which preserve the hip joint, including decompression of the femoral head augmented with concentrated bone marrow. The use of autologous stem cells has shown promise in halting the progression of AVN of the femoral head and subsequently preventing young patients from undergoing total hip arthroplasty.
Autologous bone marrow transplantation is a treatment modality in the early stages that creates the regeneration of the femoral head. Avascular necrosis (AVN) of the femoral head can be a devastating disease most commonly affecting patients younger than 40 years of age. The absence of a history of hip trauma and acute onset of deep groin pain is typical of patients who present with this condition. The development of this disease process is multifactorial, but there are accepted risk factors that have been shown to affect the relative risk of disease development. These include corticosteroid use (both amount and duration of exposure are of importance), alcohol use, smoking, hemoglobinopathy (most commonly sickle cell disease), and a variety of medical conditions(Table 1) Steroid exposure remains one of the more common risk factors. In case a series of patients receiving steroid treatments for autoimmune therapy or transplantation suppression, 10% to 30% develop AVN within 12 months of exposure. However, an idiopathic occurrence is still very common. Core decompression remains one of the most commonly used procedures in early AVN as described by Ficat and Arlet in 1964. Careful patient selection may be the most important factor in achieving success in patients who are in these so-called Pre collapse stages. Percutaneous aspiration of bone marrow stem cells from the iliac crest, and their concentration by centrifugation methods provide an autologous hematopoietic augmentation to the potential beneficial effects of core decompression. It is important to reemphasize that while the mesenchymal stem cells in the concentrated bone marrow are believed to be essential in leading to the regeneration of bone in the AVN lesions, the use of concentrated whole bone marrow, which includes other cells in the stromal and hematopoietic lineages, may also be critical to the therapeutic effect as they provide an optimized physiological and cellular environment for the promotion of both osteogenesis and angiogenesis.
Table1: Risk factors for avascular necrosis of the femoral head
Traumatic/direct injury> Femoral neck/head fracture
> Hip dislocation
> Slipped capital femoral epiphysis
Non Traumatic• Corticosteroid use
• Alcohol abuse
• Idiopathic
• Sickle cell disease
• Caisson disease
• Systemic lupus erythematosus
• Cushing’s disease
• Organ transplantation
• Prior radiation therapy
• Smoking
• Pregnancy
• Chronic pancreatitis
• Coagulopathy
• Chronic renal failure
• Lipid disorders
Recent advances in the understanding of the pathophysiology of osteonecrosis suggest that a decrease in the mesenchymal stem-cell pool of the proximal aspect of the femur might not provide enough osteoblasts to meet the needs of bone-remodeling in the early stage of the disease (10). An insufficiency of osteogenic cells could explain the inadequate repair mechanism that, it is postulated, leads to femoral head collapse. The effectiveness of bone-marrow mononuclear cells may be related to the availability of stem cells endowed with osteogenic properties, arising from an increase in the supply of such cells to the femoral head through bone-marrow implantation. Indeed, in the very early stages of osteonecrosis, providing sufficient repair capacity through the implantation of osteogenic cells could make these lesions reversible(11,12). Another possible explanation for the therapeutic effect of bone-marrow implantation is that injected marrow stromal cells secrete angiogenic cytokines resulting in
increased angiogenesis and subsequent improvement in osteogenesis. One study has suggested that the efficacy of such implantation was due to a supply of endothelial progenitor cells included in the CD34+ fraction as well as to multiple angiogenic factors (vascular endothelial growth factors, basic fibroblast growth factor, and angiopoietin-1) released from the CD34+ fractions. Thus, the outcome of osteonecrosis of the femoral head is influenced by the size of the lesion, the stage of disease, the time from the diagnosis, and etiological factors.
Promising role in Autoimmune diseases especially in Rheumatoid Arthritis
Progenitor cell applications have got a promising role in the management of Autoimmune diseases Hematopoietic stem cell transplantation has been used since 1996 for the treatment of severe autoimmune diseases refractory to approved therapies. Autoimmune diseases are a family of more than 100 heterogeneous conditions that affect 5 to 8% of the world’s population and are characterized by aberrant activation of the immune system with failure of immune regulation to maintain adapted tolerance(15) Although conventional immunosuppression and new biological agents can provide disease control in severely affected patients, such treatments are rarely curative and alternative strategies are needed.(16) Indeed, severe forms of systemic autoimmune diseases, such as multiple sclerosis (MS), systemic sclerosis (SSc), rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), juvenile idiopathic arthritis (JIA), hematologic immune cytopenia (HIC) and Crohn’s disease are difficult to treat. Hematopoietic stem cell transplantation (HSCT) is a complex multistep procedure involving mobilization and harvesting of autologous hematopoietic stem cells (HSCs) from autologous bone marrow, followed by administration of HSCs in Rheumatoid arthritis patients. HSCT has been shown to induce profound alterations of the immune system affecting B and T cells, monocytes, and natural killer and dendritic cells, resulting in the elimination of autoantibody-producing plasma cells and in the induction of regulatory T cells. The introduction of effective biologicals for the treatment of rheumatoid arthritis (RA), juvenile idiopathic arthritis (JIA), ankylosing spondylitis, and systemic lupus erythematosus (SLE) has reduced the demand for intensive and toxic treatments such as HSCT. But those cases not responding to DMRDs or Biological are the ideal cases for HSCT. Acc0rding to a study done by ACR after HSCT relapses are also there at later date and then the support of DMRDs is being taken. In some cases, good remissions of disease were there. Interestingly, sensitivity to DMARDs seemed restored after HSCT.
Conclusion
This promising new approach of stem cell therapy, for the treatment of various orthopaedic disorders, could benefit from the recent advances made in the field of stem-cell biology, including the use of subpopulations of progenitors with greater therapeutic potential. Stem cell therapy in OA knee, AVN head of Femur although still at a developmental stage and not without hurdles, promises to bring hope and eventual solution to these patients. Because bone marrow is known to contain osteogenic progenitors, its implantation was perceived to have the potential to lead to effective bone regeneration various preclinical investigations, and clinical studies, have confirmed this (17.18)Thus, Regenerative science holds a positive future in treating certain orthopaedic conditions which faces a lot of challenges in presently available treatment modalities. The potentials for using osteogenic stem cells and biomaterials in orthopedics for skeletal healing is immense, and work in this area is likely to expand significantly in the future.
References
1 Muschler GF, Nakamoto C, Griffith LG: Engineering principles of clinical cell-based tissue engineering. J Bone Joint Surg Am 86-A:1541-1558, 2004
2. Zuk PA, Zhu M, Mizuno H, et al: Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng 7:211-228, 2001
3. Agung M, Ochi M, Yanada S, et al: Mobilization of bone marrow-derived mesenchymal stem cells into the injured tissues after intraarticular injection and their contribution to tissue regeneration. Knee Surgery, Sports Traumatology, Arthroscopy 14:1307-1314,2006
4. Izuta Y, Ochi M, Adachi N, et al: Meniscal repair using bone marrow-derived mesenchymal
stem cells: an experimental study using green fluorescent protein transgenic rats. Knee 12:217-223, 2005
5. Yamasaki T, Deie M, Shinomiya R, et al: Meniscal regeneration using tissue engineering with a scaffold derived from a rat meniscus and mesenchymal stromal cells derived from rat bone marrow. Journal of Biomedical Materials Research Part A 75:23-30, 2005
6. Murphy JM, Fink DJ, Hunziker EB, et al: Stem cell therapy in a caprine model of osteoarthritis. Arthritis & Rheumatism 48:3464-3474, 2003
7. Lieberman JR, Berry DJ, Mont MA, et al. Osteonecrosis of the hip: management in the 21st century. Instr Course Lect. 2003;52:337–355.
8. Mont MA, Jones LC, Hungerford DS. Nontraumatic osteonecrosis of the femoral head: ten years later. J Bone Joint Surg Am. 2006;88: 1117–1132.
9. Arlet J, Ficat P. Mode of onset of primary osteonecrosis of the femoral head. (Stage I. Uncomplicated). Study of 20 cases histologically verified by punch biopsy. Rev Rhum Mal Osteoartic. 1968;35:239–249. [Article in French].
10. Hernigou P, Beaujean F, Lambotte JC. Decrease in the mesenchymal stem cell pool in the proximal femur in corticosteroid-induced osteonecrosis. J Bone Joint Surg Br. 1999;81:349-55.
11. Inoue A, Ono K. A histological study of idiopathic avascular necrosis of the head of the femur. J Bone Joint Surg Br. 1979;61:138-43.
12. Hauzeur JP, Pasteels JL. Pathology of bone marrow distant from the sequestrum in nontraumatic aseptic necrosis of the femoral head. In: Arlet J, Mazières B, editors. Bone circulation and bone necrosis. Berlin: Springer; 1990. p 73-6.
13. Tateishi-Yuyama E, Matsubara H, Murohara T, Ikeda U, Shintani S, Masaki H, Amano K, Kishimoto Y, Yoshimoto K, Akashi H, Shimada K, Iwasaka T, Imaizumi T; Therapeutic Angiogenesis using Cell Transplantation (TACT) Study Investigators. Therapeutic angiogenesis for patients with limb ischemia by autologous transplantation of bone-marrow cells: a pilot study and a randomised controlled trial. Lancet. 2002;360:427-35.
14. Hernigou P, Lambotte JC. Bilateral hip osteonecrosis: influence of hip size on
the outcome. Ann Rheum Dis 2000;59:817–21.
15. Davidson A, Diamond B. Autoimmune diseases. N Engl J Med. 2001;345(5):340-50.
16. Sykes M, Nikolic B. Treatment of severe autoimmune disease by stem-cell transplantation. Nature. 2005;435(7042):620-7.
17. Tiedeman JJ, Connolly JF, Strates BS, Lippiello L. Treatment of nonunion by percutaneous injection of bone marrow and demineralized bone matrixL an experimental study in dogs. Clin Orthop 1991;268:294–302.
18. Paley D, Young MC, Wiley AM, Fornasier VL, Jackson RW. Percutaneous bone marrow grafting of fractures and bony defects: an experimental study in rabbits. Clin Orthop1986;208:300–12.